Understanding Endometriosis
Learn more about endometriosis, its common symptoms, and how it is treated.
Endometriosis is one of the most common gynecological disorders, affecting approximately 10% of all women in their childbearing years2,3
It's not clear why endometriosis occurs, but we can help you understand what happens in your body. Endometriosis occurs when the endometrial lining normally found inside the uterus begins to grow outside the uterus. These growths are called lesions. They may grow on the ovaries, fallopian tubes, or other areas near the uterus. The lesions can bleed and break down each cycle, causing scar tissue and adhesions (scarring that binds tissues together).2,4
Where can endometriosis occur?2,4
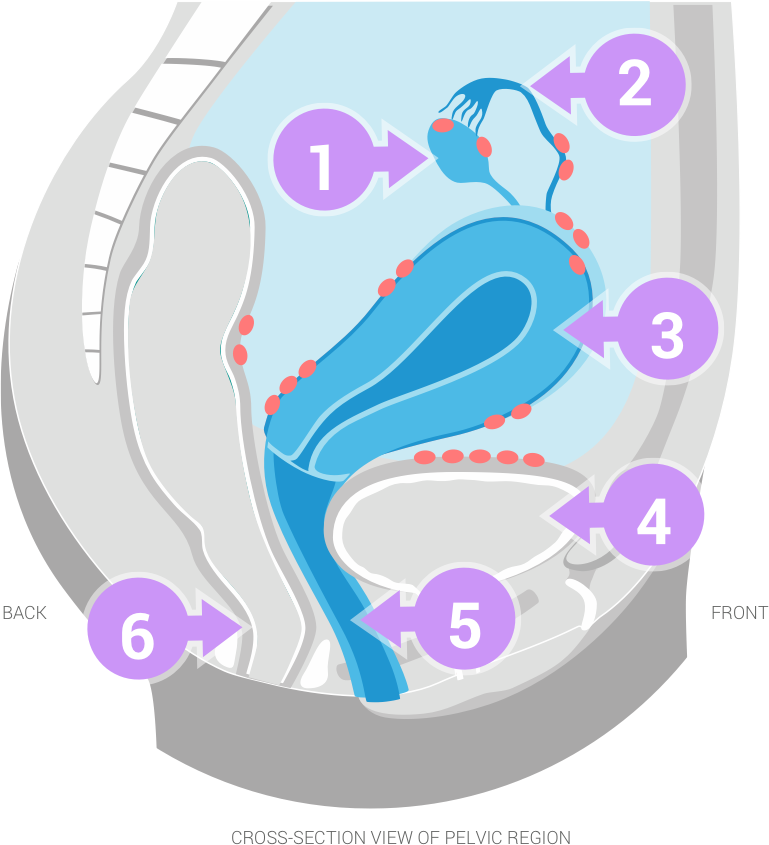
= Endometrial lesions
1. Ovary
2. Fallopian tube
3. Uterus
4. Bladder
5. Vagina
6. Rectum
Endometrial tissue builds up in the uterus every cycle, but when it grows outside the uterus, it can cause painful symptoms4
Hormones, such as estrogen, can stimulate the growth of endometriosis. When endometrial tissue grows outside the uterus, it reacts to cyclic changes in hormones, but doesn’t necessarily respond the same way normal endometrial tissue inside the uterus does. Unlike the lining inside the uterus that sheds and leaves the body with each menstrual period, endometrial tissue can grow, bleed, and possibly form scar tissue on areas outside the uterus.2,4,5
These events can cause painful endometriosis symptoms, such as4,5:
- Recurring pelvic pain
- Painful intercourse
- Painful and/or heavy periods
Many women with endometriosis have no symptoms.4
How endometrial lesions grow2,4,5
Hormones, including estrogen, are released by the ovaries.
Estrogen causes endometrial tissue to grow.
Endometrial tissue growth can lead to painful symptoms and scarring.
Treatment Considerations
Surgically
Patients with endometriosis may have a surgery called a laparoscopy to diagnose and/or treat their endometriosis. This procedure enables your doctor to examine the condition of the patient's reproductive organs and look for locations of endometriotic lesions. The doctor may also take a tissue sample called a biopsy to confirm the diagnosis.2
During the surgery, a doctor will often remove endometriotic lesions by excision (cutting) or laser ablation (dissolving them with a laser). However, some endometriotic lesions may be hard for doctors to see due to their size, location, or depth, and the patient could continue to experience endometriosis pain.2,6,7
Medically
Many women who have endometriosis initially go to their doctors because of chronic pelvic pain. Your doctor may initially prescribe medications such as contraceptives (OCs) or nonsteroidal anti-inflammatory drugs (NSAIDs) to treat that pelvic pain after ruling out other causes, such as infections.4,5,8
After confirming a diagnosis of endometriosis, your doctor may decide that a gonadotropin-releasing hormone agonist (GnRHa) medication such as LUPRON DEPOT may help relieve your pain.1,5
What is LUPRON DEPOT?
LUPRON DEPOT is a prescription medication for the management of endometriosis, given as an injection by a healthcare professional. It can help relieve the pain of endometriosis and reduce endometriotic lesions.1 LUPRON DEPOT has been prescribed by doctors since 1990.9
LUPRON DEPOT offers 2 different dosing options for treatment, both of which can be combined with Add-back* therapy from day 1 in appropriate patients1:
- Injected once every 3 months (11.25 mg dose)
- Injected once each month (3.75 mg dose)
How does LUPRON DEPOT work?
LUPRON DEPOT suppresses the hormones that cause endometrial tissue to grow.1
LUPRON DEPOT therapy suppresses the signals from the pituitary gland in the brain to the ovaries, which stimulate estrogen production.1 By doing this, LUPRON DEPOT injections also suppress the hormones that cause endometriosis to grow. Suppressing the hormones helps1,4:
- Provide endometriosis pain relief
- Reduce endometriotic lesions
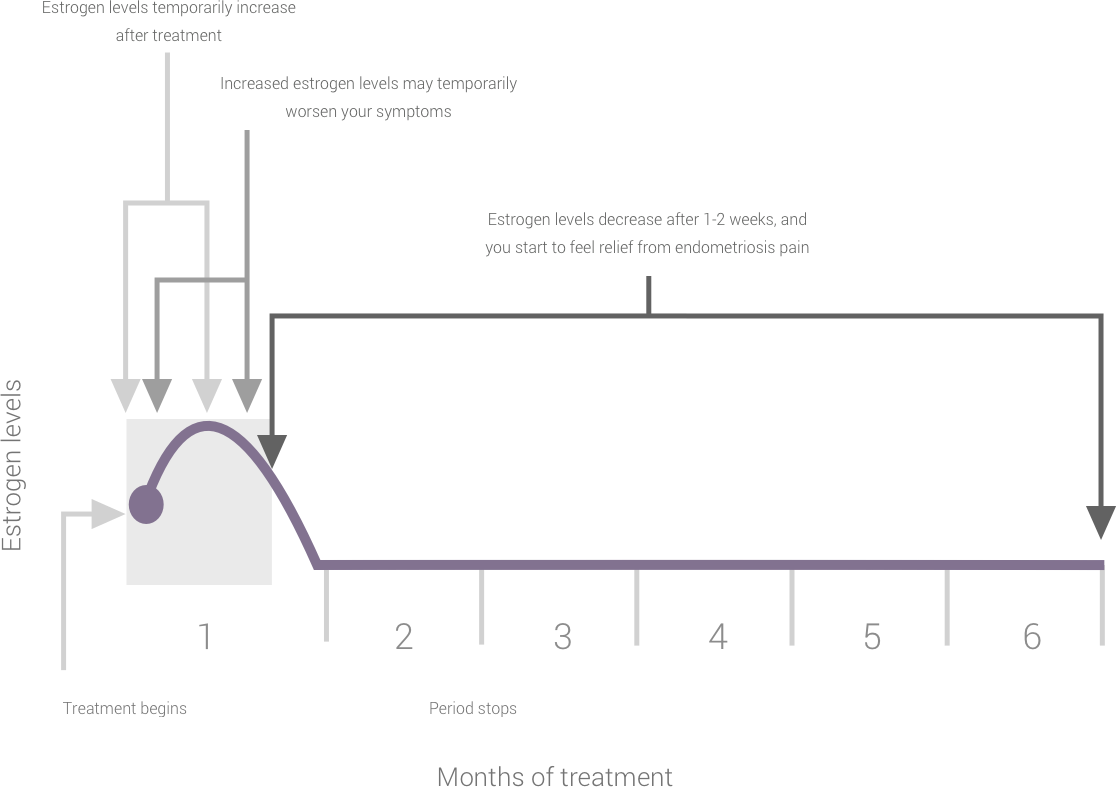
What can you expect during a 6-month course of LUPRON DEPOT therapy?1,5,10
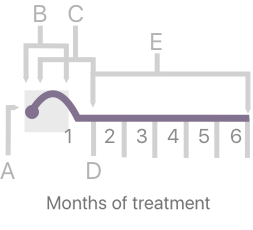
For illustrative purposes only. Responses may vary in individual patients.
Since ovulation and menstruation usually stop with effective doses of LUPRON DEPOT, you should notify your doctor if regular menstruation persists. If you miss successive doses of LUPRON DEPOT, you may experience breakthrough bleeding. You should notify your doctor immediately if you develop any new or worsened symptoms after beginning LUPRON DEPOT.1
Things to keep in mind
Your estrogen levels will increase for 1 or 2 weeks after beginning LUPRON DEPOT. During this time, you may notice an increase in your current symptoms. You should notify your doctor if you develop any new or worsened symptoms after beginning LUPRON DEPOT treatment.1
LUPRON DEPOT is not a method of birth control. Even though you may not have a period, unprotected intercourse could result in pregnancy. You should use non-hormonal birth control such as condoms, a diaphragm with contraceptive jelly, or a copper IUD to prevent pregnancy. Contact your doctor immediately if you think you may be pregnant.1
Who should not take LUPRON DEPOT?
You should not receive LUPRON DEPOT if you1:
- Are or may become pregnant
- Have undiagnosed vaginal bleeding
- Have experienced any type of allergic reaction to LUPRON DEPOT, or similar drugs
- Also do not take LUPRON DEPOT 3.75 mg if you are breastfeeding
You should not receive Add-back* plus LUPRON DEPOT if you have or have had any of the following conditions1:
- Clotting disorder
- Stroke
- Impaired liver function or liver disease
- Breast cancer
Endometriosis pain relief and lesion reduction with LUPRON DEPOT.
LUPRON DEPOT can help reduce endometriosis pain1
By suppressing the hormones that feed endometriosis, LUPRON DEPOT injections can help reduce your endometriosis pain and reduce the size of endometriotic lesions. In 2 studies of women undergoing endometriosis treatment with LUPRON DEPOT 3.75 mg for 6 months, 96% of women had relief from painful periods after their initial 6 months of therapy. Many also experienced relief from painful intercourse, pelvic tenderness, and pelvic pain.1,11
Study Design
One hundred and twenty-five patients from two 6-month, double-blind, randomized clinical studies entered a 1-year follow-up study. This study grouped patients who received 3.75 mg LUPRON DEPOT during previous trials and assessed recurrence of endometriosis signs and symptoms and safety parameters after discontinuation of treatment. The primary endometriosis signs and symptoms assessed were dysmenorrhea (painful periods), non-menstrual pelvic pain (NMPP) (pain in the pelvic area before or after periods), dyspareunia (pain during sex), pelvic tenderness (pain during the pelvic examination), and induration (hardening of pelvic tissues). The first day of the study was considered to be 29 days after the final study injection. Return of pain was defined to have occurred during the month for which pain levels returned to baseline (prior to treatment) levels or worse. At each study visit, an evaluation was made of dysmenorrhea, NMPP, and dyspareunia by patient interview. Pelvic tenderness and induration were evaluated by pelvic examination.12
Percent of women who FOUND RELIEF
within 30 days of completing treatment with
LUPRON DEPOT
(6 months of therapy)1,11
Percent of women who FOUND RELIEF
12 months after completing treatment with
LUPRON DEPOT
(6 months of therapy)1,11
Relief from painful periods
pelvic tenderness
(hardened endometrial tissue)
Common side effects
In clinical trials, the most common side effects of LUPRON DEPOT, occurring in >10% of patients, include hot flashes/sweats, headache/migraine, decreased libido, depression/emotional lability, dizziness, nausea/vomiting, pain, vaginitis, and weight gain.1
About Add-back* therapy and side effects
When LUPRON DEPOT is used alone, bone thinning and hot flashes can occur. Along with LUPRON DEPOT injections, your doctor may prescribe Add-back* therapy. Add-back* is a daily pill that you take while on LUPRON DEPOT therapy to add back a small amount of the hormone progestin, which can help you manage certain side effects, without interfering with the way LUPRON DEPOT works.1,5
Add-back* may be prescribed from Day 1 of initial treatment with LUPRON DEPOT. Add-back* is not for everyone and should not be taken by women who currently have or have had any clotting disorder, heart disease, stroke, impaired liver function or liver disease, or breast cancer.1
*Norethindrone acetate 5 mg daily.1
What can you expect after discontinuing LUPRON DEPOT?
- After completion of a full course of treatment with LUPRON DEPOT therapy, the hormonal effects you may have experienced should subside.1
-
Your normal menstrual cycle should return. The amount of time for your menstrual cycle to return is different for each woman.1
- In one study of 166 patients treated with LUPRON DEPOT 3.75 each month for 6 months, 95% of women resumed their cycle within 3 months after completion of therapy.1
- Bone loss might not be completely reversible in some patients. Since some conditions may increase the possibility of bone thinning, you should tell your doctor if you smoke, use alcohol heavily, have a family history of osteoporosis (thinning of the bones with fractures), or are taking other medications that cause thinning of the bones.1
Educational brochure
Learn about LUPRON DEPOT for endometriosis.